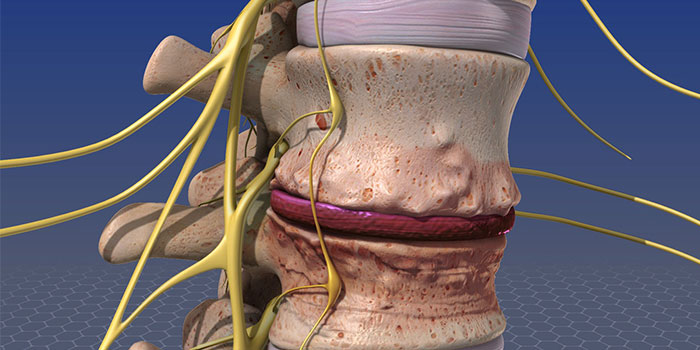
A spinal infection is a rare, but often serious, form of disease that occurs when bacteria, fungi, or viruses invade the spinal tissues. These foreign agents can attack pretty much any part of the spine that you can image. This includes the vertebrae, spinal discs, meninges, spinal canal… and even the spinal cord.
When these pathogens infect our intervertebral discs, doctors refer to this condition as Discitis, or disc inflammation. When these bugs attack the bones of our spine, we refer to the disease as Osteomyelitis.
Typically, these infections spread to the spine through the bloodstream. Common bacteria, like Staph or E. Coli, can be introduced into the bloodstream following events such as surgery or drug abuse.
Any event that introduces bacteria into the bloodstream or that weakens the immune system can lead to a spinal infection. For example, those who take immunosuppressants (whether following an organ transplant or to treat an autoimmune disease) often suffer from secondary infections. These can be mild, like a simple cold, or very serious, like osteomyelitis.
In addition, if you have recently undergone spine or pelvic surgery, then your risk of contracting a spinal infection rises steeply. This is true for two reasons. Firstly, surgical instruments and medical devices can introduce germs into the body if they are not properly sterilized. Secondly, your Batson’s plexus (a network of blood vessels) connects your thoracic veins to your pelvic veins, bladder, and prostate. If bacteria from any of these areas infiltrates the plexus, then you can develop a spinal infection.
Via the Batson’s plexus, infections from the bladder (urinary tract infections) or the prostate can also spread to the spine. The risk of developing a secondary spinal infection from a UTI increases tenfold, for example, following a urologic procedure, like a scope.
Infections, like pneumonia and tuberculosis, can also spread to the spine from the lungs. Other diseases that enhance your risk of developing a spinal infection include diabetes, cancer, HIV, and malnutrition. Other events that increase your risk include intravenous drug use, long-term use of steroids, and spinal trauma.
The symptoms of a spinal infection tend to develop very slowly. For example, it may take you a week to realize that you’re coming down with a cold. In contrast, spinal infections take between 3 days and 3 months to notice, with an average of a month and a half before detection. Common warning signs of a spinal infection include:
Standard treatment options for spinal infections include: Intravenous Antibiotic Medications: To kill the infection, antibiotics may be prescribed for anywhere from 7 to 10 days, to 6 to 12 weeks. A central line may need to be placed in order to assist in the administration of longer-term medications.
Copyright © All Rights Reserved, By Shethna Spine Clinic